Intervertebral Hernia – What Is It?
In terms of economic impact on society, back pain ranks third after heart and cancer diseases. It accounts for up to 76% of all cases seeking medical help.
Intervertebral disc hernias are quite dangerous and complex diseases of the musculoskeletal system and are the most common causes of back pain as well as discomfort in the pelvic region and legs. In Europe alone, doctors diagnose about half a million cases of this disease annually, and this number continues to grow. Hernias occur in people of all age groups and both sexes.
The disease arises due to the protrusion of the intervertebral disc, which presses on nearby nerve endings and spinal nerve roots. The pinched nerve root sends pain impulses to the brain, which the person perceives as pain in the area served by that nerve. The substance of the nucleus pulposus acts as a chemical irritant to the nerve tissue, contributing to the development of local inflammation, swelling, and microcirculatory disorders. This causes local irritation of sensitive receptors and muscle spasms, leading to restricted mobility in the affected area (a reflex mechanism). Prolonged spasms lead to posture impairment, development of pathological motor stereotypes, and maintenance of the pain syndrome.
However, the pain caused by an intervertebral hernia is not the worst outcome. This disease can provoke dysfunction of internal organs, loss of sensitivity in various body areas, and, consequently, paralysis of the arms and legs.
By the cause of their occurrence, all intervertebral hernias are divided into primary and secondary.

Primary hernias are those that arise suddenly due to heavy physical exertion or trauma during which the intervertebral discs get damaged.
People who frequently perform intense physical work, as well as those whose jobs involve heavy lifting (athletes, loaders, miners, construction workers, etc.), are in the main risk group.
One awkward movement with a barbell or another heavy load in hand can cause the intervertebral disc to shift to the side or crack. Unfortunately, even the most experienced athletes, who know all the intricacies of working with heavy sports equipment, are not immune to this problem.

Secondary hernias are the result of the development of various diseases of the musculoskeletal system. There are many spinal diseases that can lead to the appearance of a hernia, but the undisputed leader among them is osteochondrosis.
Bad habits also negatively affect the intervertebral discs of the spine, thereby stimulating the formation of hernias. Smoking reduces the oxygen saturation of the blood, depriving the spinal discs of vital elements. Coffee consumption worsens blood circulation in the surrounding spinal tissues, and irregular nutrition also negatively affects the spine.
A sedentary lifestyle also provokes the development of hernias. If you spend a lot of time sitting behind the wheel or at the computer, leading a sedentary lifestyle, there is a high chance that sooner or later you will face this disease.
When treating intervertebral hernias, it is important not to miss the moment when conservative methods can still help and avoid surgery with all its consequences. With timely consultation with a specialist, progression can be stopped and possible complications prevented.
By location, hernias are classified as follows:
Thoracic hernia (4%) – occurs in people over 35-40 years old and after injuries. May cause pain in the thoracic spine area, pain during inhalation and exhalation, chest pain when bending, blood pressure fluctuations, and difficulty straightening the back.
Lumbar-sacral hernia (65%) – the most common due to the heavy load on this section. Causes dull and sharp pain in the lower back, numbness, sweating disturbances, coldness in the legs, urinary incontinence or retention, constipation, diarrhea, erectile dysfunction in men, menstrual cycle disruptions in women, and in advanced stages may cause paralysis.
Cervical hernia (31%) – dangerous due to the possibility of vertebral artery compression. Characterized by neck pain radiating to the shoulder blade or arm, frequent headaches, dizziness, muscle weakness, decreased sensitivity of the skin and muscles of the face and arms, often causes vision deterioration, hearing loss, hoarseness, and snoring.
Most intervertebral hernias form in the lumbar region, which bears the greatest load (150 cases per 100,000 population per year), and in the cervical spine, which is the most mobile. In the vast majority of cases, intervertebral disc hernia is a staged process—from minimal clinically unrecognized displacements to fibrous ring tears with severe symptoms.
 |  |  |
In this regard, hernias are classified BY THE VOLUME OF PROTRUSION:
PROLAPSE – protrusion of 2-3 millimeters; at this stage, symptoms often are absent because metabolic disturbances have not yet caused structural changes in the disc.

• PROTRUSION – protrusion from 4-5 up to 15 millimeters. Due to irritation of nerve roots, radicular pain appears. The displaced nucleus does not extend beyond the boundaries of the fibrous ring.
• EXTRUSION – the displaced nucleus presses on the fibrous ring and moves beyond the disc. Displacement most often occurs posteriorly or posterolaterally – into the spinal canal. This causes persistent pain syndrome with muscle atrophy in the innervated area.
• SEQUESTRATION – the displaced nucleus hangs outside the disc like a drop. This often results in a rupture of the fibrous capsule with leakage of the gelatinous nucleus and the formation of ankylosing spondyloarthrosis.
It is important to discuss the size of intervertebral hernias together with their localization. The size of a small hernia in the lumbar spine can be critical in the cervical spine.
CLASSIFICATION OF HERNIAS IN LUMBAR AND THORACIC REGIONS:
- SMALL: size less than 5 mm.
- MEDIUM: size from 6 to 8 mm.
- LARGE: size from 9 to 12 mm.
- PROLAPSE/SEQUESTRATION: size over 12 mm.
CLASSIFICATION OF HERNIAS IN CERVICAL REGION:
- SMALL: size less than 2 mm.
- MEDIUM: size from 3 to 4 mm.
- LARGE: size from 5 to 7 mm.
- PROLAPSE/SEQUESTRATION: size over 8 mm.
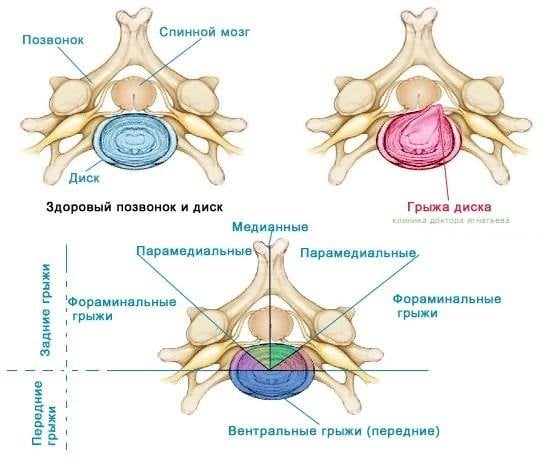
The clinical picture and severity of the disease also depend on the part of the fibrous ring where the rupture occurred.
TYPES OF INTERVERTEBRAL HERNIAS BY DIRECTION OF PROTRUSION:
- LATERAL – hernias exit from the side of vertebral bodies, often through the openings for spinal nerve roots.
- POSTERIOR – hernia directed inward into the spinal canal, causing so-called cauda equina syndrome. This type is the most severe and dangerous.
- POSTEROLATERAL – the most common type of spinal hernia, subdivided into:
- FORAMINAL HERNIAS – protrusion directed toward the intervertebral foramen, compressing nerve endings passing through it.
- DORSOLATERAL – posterolateral disc protrusions, especially dangerous in the cervical spine due to risk of artery compression.
- ANTEROLATERAL – protrusion develops forward and causes no symptoms; considered the most favorable type.
- MEDIAN – also directed inward into the spinal canal and compress it on one or both sides in the middle.
- COMBINED
The most problematic are posterior and posterolateral disc protrusions into the spinal canal. In such cases, pain and sensory disturbances are usually accompanied by dysfunction symptoms of internal organs: heart, stomach, intestines, urinary system.
BY POSITION RELATIVE TO THE MIDLINE, HERNIAS ARE:
- MEDIAN
- PARAMEDIAN
- LATERAL
DISEASE PROGRESSION STAGES:
- INITIAL STAGE – a crack appears in the fibrous ring and contents begin to protrude, the nucleus gradually bulges, causing shooting pain.
- PARTIAL PROLAPSE – pain becomes constant, swelling appears near the nerve root, and blood supply is disrupted in the disc area.
- FULL PROLAPSE – pain intensifies and radiates into the lower limbs. Disability is possible.
- SEQUESTRATION – disc fragments displace and several nerve roots are affected simultaneously, leading to pulsating and debilitating pain.
ANATOMICAL STRUCTURE CLASSIFICATION OF HERNIAS:
- FREE – the structure is still connected to the intervertebral disc.
- MIGRATING or SEQUESTERED – completely lose connection to the damaged disc; these hernias move within the spinal canal and pose a risk of nerve compression.
- DISPLACED – the hernia shifts and sometimes returns to place.
Diagnosis is made by an orthopedist or neurosurgeon based on symptoms. To clarify the diagnosis, the following methods are used: CT scan, spondylography, X-ray. Examination and treatment must not be delayed. Specialists at dedicated Clinics of Vertebrology, Orthopedics, and Traumatology can provide diagnosis and professional treatment courses.