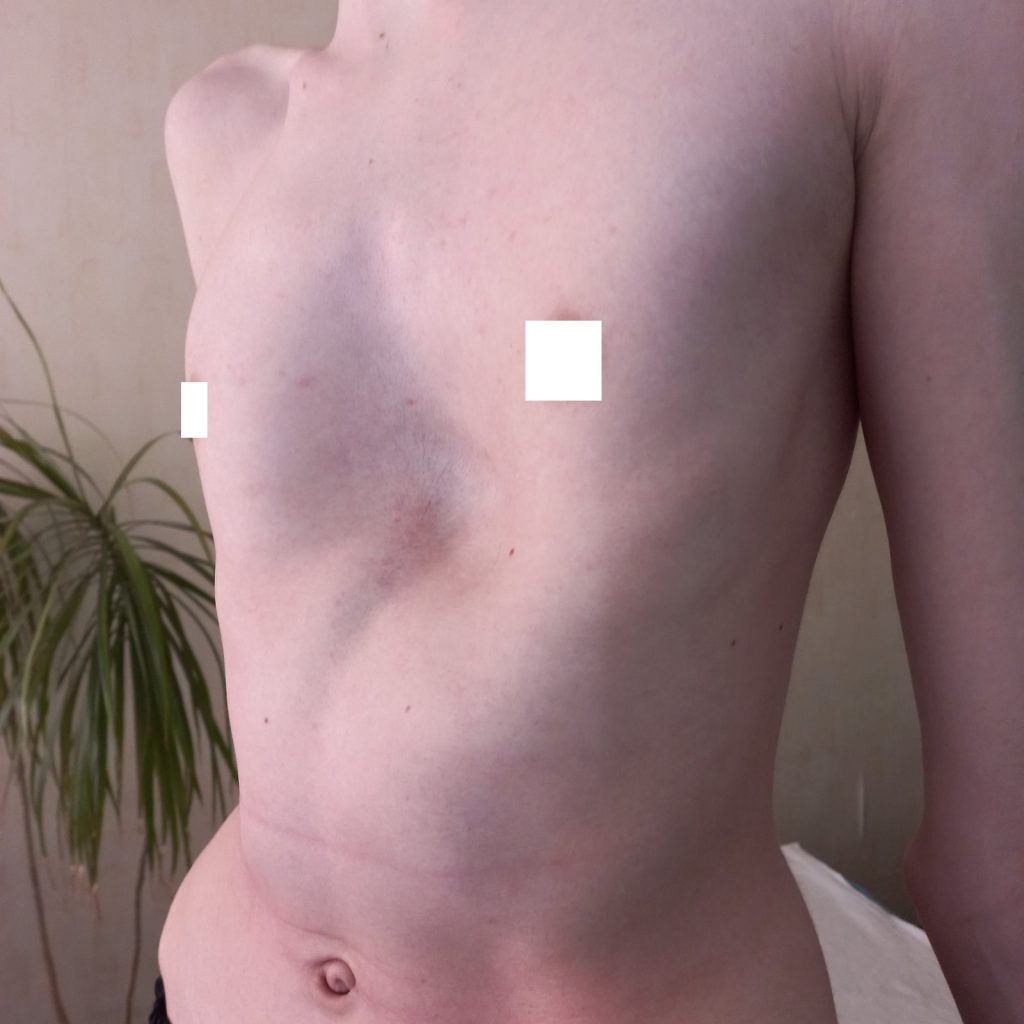



According to statistics, approximately one in 1,000 children is born with a chest deformity known as “shoemaker’s chest,” which manifests as a funnel-shaped deformity of the chest and is sometimes accompanied by rib retraction. In most cases, this defect affects the development and function of internal organs (lungs and heart) and is accompanied by an impaired aesthetic appearance of the chest. It is the most common chest deformity (91% of all congenital chest defects). This defect is more noticeable and occurs more frequently (70%) in males. The chest deformity is more common in slender boys. Girls are also affected, but as they grow older and develop breasts, the defect becomes less noticeable.
Funnel chest (pectus excavatum, s. infundibuliform) was first described by Bauhinus in 1600 but was more thoroughly detailed in Eggel’s work (1870). The causes of its development have not been definitively established, but many authors indicate that the deformity has a pronounced congenital character; it is associated with dysplastic changes of the cartilage and connective tissue of the chest, often has a familial character, i.e., a genetic factor, and the tendency to progression is well justified.
Clinically, three stages of the disease are distinguished:
- compensated
- subcompensated
- decompensated
In the compensated stage, patients with chest deformity have only a cosmetic defect; complaints and functional disorders are absent.
In the subcompensated stage, pronounced functional disorders of the lungs and cardiovascular system are often detected.
CAUSES OF THE PATHOLOGY
It is impossible to predict in advance who and when will be affected, as the causes of the disease are still not fully understood. According to one theory, in 25% of cases, the cause may be genetic predisposition, and the “source” can come not only from the mother and father but also from grandparents.
There is another opinion. The chest of the fetus forms during the 6th to 10th weeks of pregnancy, and if during this period the mother experienced illness, stress, or even consumed something harmful (for example, alcohol), intrauterine development may be disrupted, and one of the consequences of this disruption could be chest deformities. However, these remain just theories for now. Since the cause of the condition is unknown, there are no known methods for its prevention.

Clinical chest deformity depends on the child’s age:
IN INFANTS, the deformity often appears in the first months after birth as a slight indentation. A characteristic sign in this age group is the “paradoxical breathing” symptom (sunken sternum and ribs during inhalation). It may manifest only as paradoxical breathing and less commonly as stridor due to tracheal compression and displacement by the heart, or dysphagia symptoms (regurgitation and vomiting after feeding). It is most noticeable when the baby cries or screams. It is difficult to predict the progression of the deformity in infants. According to our data, in almost half of the cases, the indentation increases with growth, the chest depression becomes more noticeable. The edges of the costal arches begin to protrude, and a transverse groove forms above them (pseudo-Harrison’s groove). These changes are sometimes mistakenly considered signs of rickets. In Ukraine, for example, a pronounced chest deformity is grounds for recognizing a child as disabled.
IN PRESCHOOL CHILDREN, there is a gradual transition to fixed curvature of the sternum and ribs, posture changes, and thoracic kyphosis intensifies; on examination, the child shows drooping shoulders and elevated edges of the costal arches. At this age, funnel chest usually does not represent a serious cosmetic defect, but changes in the lungs and heart become more pronounced, with a tendency to frequent colds. Deformation-induced changes become more evident with age. The child lags in weight and physical development; the abdomen protrudes forward, posture disorders develop in the form of scoliosis and kyphosis, vision problems, dental caries, flat feet, pale skin, and biliary and intestinal dyskinesia manifesting as unstable stools with diarrhea and constipation.
IN SCHOOL-AGED CHILDREN (7-9 years — the first period of active growth), chest deformity and posture disorders progressively worsen; these children are often undernourished with pale skin, fatigue quickly during walking and running, experience shortness of breath and palpitations during physical exertion, chest pains, irritability, poor appetite, frequent respiratory infections, tonsillitis, bronchitis, and pneumonia. Due to the chest defect, lung ventilation is impaired, and infections develop easily in the context of congestion. A child may catch a cold like others, but an ordinary cold more often develops into bronchitis or pneumonia.
The deformity becomes fixed, chest excursion decreases, and vital lung capacity reduces by 18-30% (instead of four liters normally, about three and a half liters). Children with sternum deformity may lag behind their healthy peers in sports and physical activities. Patients show altered external respiration parameters and cardiovascular function. Pressure of the sternum on the heart causes its displacement, rotation, and arrhythmias. In severe funnel chest, spinal curvature, changes in venous and arterial pressure, thoracic kyphosis often combined with scoliosis are observed. Increased fatigue, sweating, irritability, decreased appetite, pale skin, and weight loss compared to age norms are noted.
Besides somatic complaints, children develop an inferiority complex, as the chest deformity becomes noticeable to others, especially classmates.
PSYCHOLOGICAL IMPACT
Children with sternum defects or spinal curvature often feel ashamed of their appearance. They may avoid changing clothes in front of others during PE lessons, avoid swimming pools, and avoid sunbathing at the beach. Meanwhile, if treatment is started timely and properly, the deformity can often be corrected.
IN ADULTS, regarding military service, studies in many countries have assessed the suitability of people with chest deformities for service. US scientists found that sternum defects disrupt the heart’s electrical conduction and reduce its pumping function.
HOW IS CHEST DEFORMATION TREATED?
Treatment of funnel chest is carried out by traumatologists, orthopedists, and thoracic surgeons. Because of its tendency to progress, funnel chest sometimes poses a serious health risk.
Conservative treatment of funnel chest is ineffective. Exercises and massages are helpful for all children but do not correct the deformity. However, children with chest defects should definitely engage in physical activity to improve heart and lung function.
Surgical treatment is indicated for organ dysfunction in the chest or significant cosmetic defects. The optimal age for surgery is preschool (3-7 years), as the body can still compensate for pathological changes in internal organs, and children do not suffer psychological trauma regarding their appearance. This approach allows proper chest formation, prevents secondary spinal deformities, and functional disorders. Moreover, children tolerate surgery better, their chest wall is more elastic, and correction is less traumatic.
NUSS OPERATION
Recently, at the Galaxia Clinic in the Center for Spine and Chest Deformity Correction and Pain Therapy, the American method by Donald Nuss was introduced. This is one of the safest and most effective minimally invasive methods for correcting chest deformities. Today, this method is well established worldwide and has no current alternatives in terms of effectiveness and safety.



WHAT DOES THE METHOD CONSIST OF?
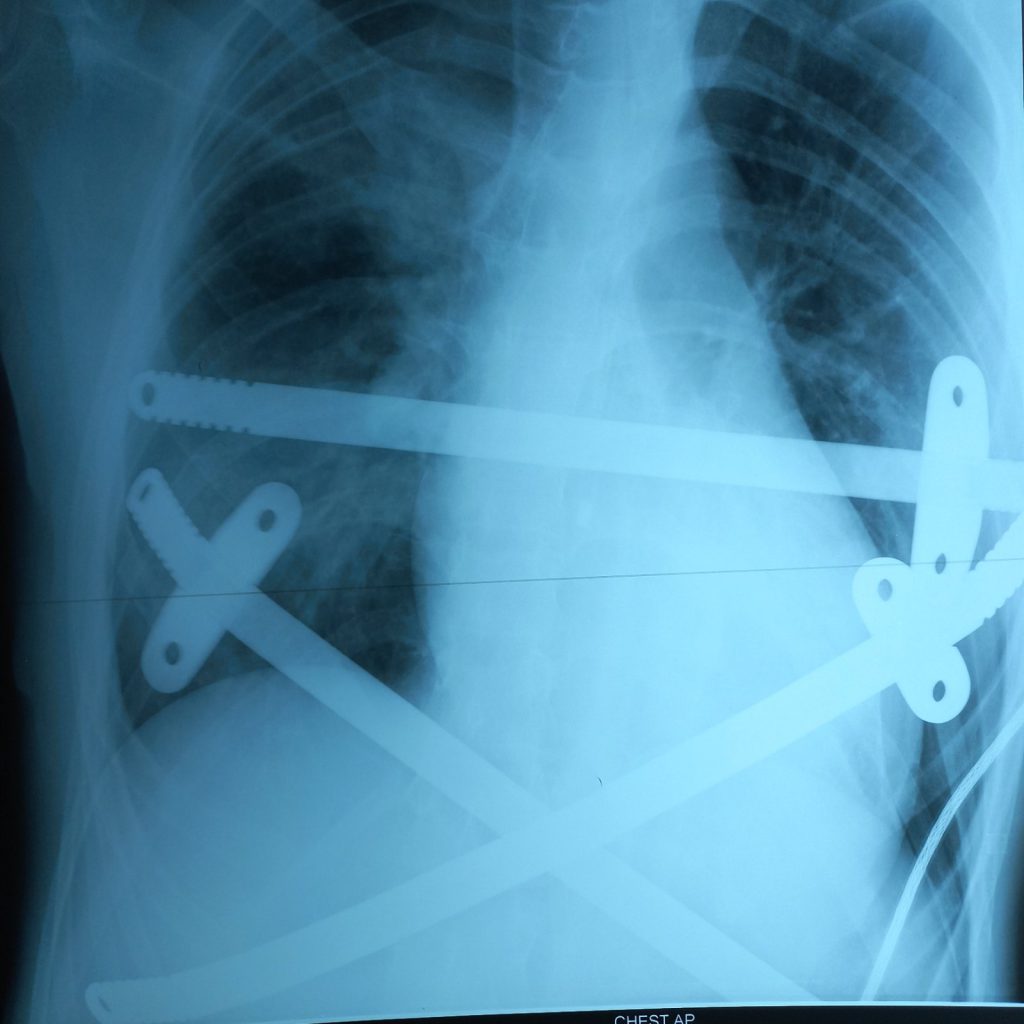
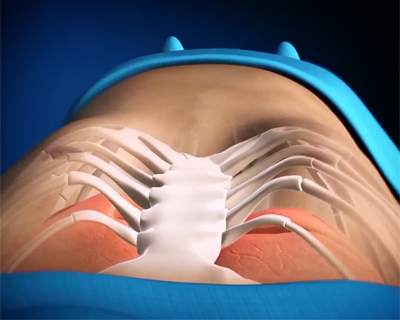
The method involves implanting a metal bar that helps straighten the chest. The operation is performed under general anesthesia. The patient is placed with both arms raised to allow access to the lateral chest wall. A transverse incision about 2.5 cm long is made on each side of the chest, between the anterior and posterior axillary lines. A curved clamp is passed through the mediastinum until it appears on the opposite side.
Using a traction tape, a pre-shaped steel bar is pulled through. The bar, with its convexity facing backward, is passed under the sternum. When the bar is in place, it is rotated with clamps so that the convexity faces forward, thereby lifting the sternum and the anterior chest wall into the desired position. If needed, a second bar is placed either above or below the first. If the bar is unstable, a crossbar 2-4 mm long is attached to one or both ends of the bar. If two bars are used, crossbars are attached to both ends to form a rectangle. The wounds are sutured layer by layer.
Approximately after 3 years, the bar is removed through the same incisions used during implantation. After removal, the patient is considered fully healthy, and the chest deformity corrected.
Furthermore, doctors note that complications caused by the Nuss procedure are minimal, and the patient’s recovery period is significantly shortened.
Patient satisfaction with the results is very high (up to 98%), with only about 2% having residual deformity, mostly due to deviations from the surgical technique during the creation of the retrosternal tunnel. Major advantages of the method include its minimally invasive nature, shorter rehabilitation compared to older chest deformity correction surgeries, and the absence of noticeable postoperative scars since small incisions on the sides are used to fully correct the deformity.
POST-OPERATIVE RESTRICTIONS
Like with any surgery, there are restrictions to be followed for 3-4 months:
- Sleep on your back only. Avoid sleeping on your side or stomach. It’s recommended to use an orthopedic pillow.
- Avoid sudden movements.
- No sports activities.
- Do not lift heavy objects.
- Avoid falls (especially important on icy surfaces).
- Try to avoid public transportation to prevent someone from bumping, hitting, or pushing you, as the bar can still shift.
- MRI scans are prohibited while the bar is implanted.
- If you have an accident during this period, it will be problematic because direct heart massage (CPR) may not be possible.