Transdermal Treatment of Lumbar Intervertebral Disc Hernias with Gelified Ethanol and Radiopaque Substance
Preliminary Study
Jacques Theron, MD, PhD,* Leopoldo Guimaraens, MD, PhD,† Alfredo Casasco, MD, PhD,† Teresa Sola, MD, PhD,‡ and Hugo Cuellar, MD, PhD,†
Study Design: Prospective clinical study.
Objective: To confirm the safety and effectiveness of gelified ethanol in percutaneous treatment of lumbar intervertebral disc hernias.
Background: After the market withdrawal of the drug Chymopapain, the need for new substances to treat intervertebral disc hernias became evident. Good results were obtained with pure ethanol; however, handling this substance involves certain difficulties. We decided to use the same substance mixed with ethylcellulose to increase its viscosity, additionally adding a contrast agent.
Methods: This preliminary study included 276 randomly selected patients referred for treatment of lumbar intervertebral disc hernias. These patients received treatment with gelified ethanol containing a contrast agent (GECA, radiopaque gelified ethanol, RGE) and intra-articular steroids. Three groups were identified: Group A included patients treated with GECA only; Groups B and C consisted of severe cases with a narrow canal, foraminal hernia, or hyperalgesic hernia with severe pain. In these groups, GECA treatment was combined with another interdiscal procedure—automated percutaneous discectomy in Group B and radiofrequency nucleoplasty in Group C.
Results: In Group A, of 221 patients, 202 (91.4%) showed very good or good outcomes. In Group B, 37 out of 44 patients (84%) had very good or good results, and similar results were obtained in 9 out of 11 patients (82%) in Group C. No allergic complications were observed in any of the patients. Control magnetic resonance imaging (MRI) conducted shortly after treatment showed minor or no changes in the intervertebral discs, which did not correlate with clinical symptoms. MRI performed after a longer period demonstrated significant reduction in hernia volume.
Conclusions: This preliminary study confirms the effectiveness and safety of the new substance, which may replace Chymopapain.
Keywords: disc hernia, percutaneous, gelified ethanol with contrast agent, back pain, Chymopapain, discectomy, nucleoplasty
(J Spinal Disord Tech 2007;00:000-000)
Received for publication July 14, 2006; accepted January 8, 2007.
From *Neuroradiology Department, University Hospital Center Côte de Nacre, Avenue de la Côte de Nacre, Caen, France; †Nuestra Señora del Rosario Clinic, Madrid; and ‡Main Hospital of Catalonia, Barcelona, Spain.
Reprint requests: Jacques Theron, MD, PhD, Neuroradiology Department, University Hospital Center Côte de Nacre, Avenue de la Côte de Nacre, Caen, France 14000 (Email: [email protected]). Copyright © Lippincott Williams & Wilkins.
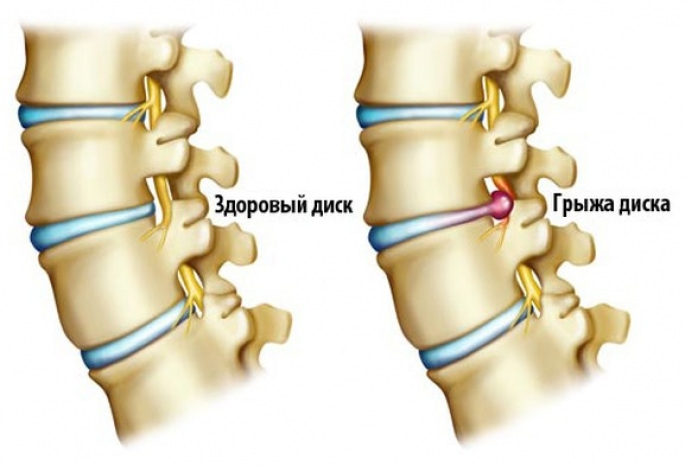
The withdrawal of Chymopapain from the market¹,² led to substantial changes in the treatment methods for intervertebral disc hernias (IDH). Based on the experience of Riquelme et al.³, we used pure ethanol (PE) for treatment, obtaining satisfactory and comparable results. However, diffusion of pure ethanol is difficult to control, and we encountered several cases of transient burning radicular pain in the leg on the injection side. We also refrain from using PE in IDH cases with epidural infiltration during discography or in thoracic or cervical IDH. This led us to replace PE with PE combined with ethylcellulose, which is used in treating venous disorders⁴,⁵ to increase its viscosity and potentially provide better diffusion control; we also added an inert contrast agent to improve visualization under fluoroscopy⁵ (Fig. 1).
This was a preliminary study in which gelified ethanol with a contrast agent (GECA) was applied as a therapeutic agent in nucleolysis for patients with lumbar IDH to confirm its effectiveness and safety.
METHODS
To evaluate the effectiveness of gelified ethanol with contrast agent (GECA) in lumbar intervertebral disc hernias (IDH), a prospective preliminary study was conducted. Approval was obtained from the hospital Ethics Committee. Patients referred for percutaneous treatment of IDH were interviewed regarding their consent to participate in the study, in which GECA was used as the therapeutic agent for nucleolysis. Informed consent was obtained.
We maintained the basic original therapeutic concept that had been used for many years when nucleolysis was treated with Chymopapain⁶:
- Concomitant intra-articular steroid injection into the adjacent facet joint for all patients.
- Application of a second intradiscal procedure for patients for whom treatment with Chymopapain would be less effective (e.g., foraminal hernias, narrow spinal canal, hyperalgesic hernia).
FIGURE 1. Treatment of lumbar intervertebral disc hernia using GECA. A. CT before treatment. B. Disco-CT after treatment, showing areas with GECA concentrated in the bulging hernia between intervertebral spaces. C. Plain radiograph after treatment showing GECA within the disc and bulging hernia.
Such a procedure was either automated percutaneous discectomy (APD)⁷, which we performed on more than 1,500 patients either alone or in combination with Chymopapain, with good results, or radiofrequency nucleoplasty (RFN).
Patients were divided into 3 groups based on the procedure applied (Table 1).
Procedures were performed under local anesthesia, in an operating room under digital fluoroscopy control, with patients lying on their right side. Discography was performed before GECA nucleolysis in groups A and B. In group C, discography was preferably performed after GECA nucleolysis, because the presence of contrast agent and GECA seems to reduce the radiofrequency effect, at least in vitro.
The dose of GECA ranged from 0.4 to 0.8 ml. In all cases, at the end of the procedure, a systematic intradiscal injection of 1 to 3 mg gentamicin was administered (to prevent infection). At least one facet joint at the treated level received an intra-articular injection of 20 mg triamcinolone to reduce inflammation; in cases of bilateral symptoms, injections were administered into both facet joints (20 mg each).
Three hours after the injection, all patients underwent thin-slice computed tomography (CT) of the treated region. Modified protocols allowed better visualization of the metallic powder mixed with the gel.
Patients continued to receive anti-inflammatory and analgesic medications until the final consultation, typically lasting 15 days. Treatment was adjusted depending on residual symptoms. All patients returned for follow-up consultations 6 weeks after treatment, and subsequently as needed based on symptoms.
Group A: Intradiscal injection of gelified ethanol with contrast agent (GECA) only + intra-articular steroid injection (IAS)
Group B: Intradiscal injection of GECA + automated percutaneous discectomy (APD) + IAS
Group C: Intradiscal injection of GECA + radiofrequency nucleoplasty (RFN) + IAS
RESULTS
A total of 276 randomly selected patients with lumbar intervertebral disc hernias were included in the study. One hundred sixty patients were male (58%) and 116 were female (42%), aged between 19 and 83 years (mean age 45.9). An overview of patient symptoms is presented in Table 2. All patients had clinical symptoms persisting for 3 months (except for 8 patients with acute hyperalgesic hernias accompanied by severe pain). All patients had received conventional treatments (anti-inflammatory drugs, local steroid injections, etc.) with no improvement.
Group A included 221 patients (Figures 1-4). One hundred forty-eight patients were treated at a single level (L2/L3: 7 cases; L3/L4: 19 cases; L4/L5: 56 cases; L5/S1: 66 cases), and 73 patients were treated at 2 or more levels (L4/L5 and L5/S1 in 60 cases, 82%).
Group B included 44 patients, and Group C included 11 patients. Among these two groups, 41 patients had spinal canal stenosis, 6 had foraminal hernias, and 8 had hyperalgesic hernias with severe pain. In all cases, treatment was performed at a single level (L4/L5 in 47 cases, 85%) (Figure 5). The decision to assign patients to Group B or C depended on the adequacy of the intervertebral space for safe insertion of the automated percutaneous discectomy kit.
Results were classified based on the following parameters: pain reduction, degree of disability, and ability to return to normal activities (Table 3).
- Sciatica + radiculitis: 195 (70%)
- Sciatica only: 54 (20%)
- Radiculitis only: 19 (7%)
- Hyperalgesic hernia: 8 (3%)
- Total: 276 patients
- FIGURE 2. Lumbar disc hernia causing lumbar radicular neuralgia requiring treatment. The patient underwent an intradiscal injection of gelified ethanol with contrast (GEC).
A. CT before treatment.
B. CT after treatment showing GEC behind the intervertebral space and penetrating the hernia.
C. Complementary 2-level intraarticular steroid injection (see text), with preliminary contrast injection into the 4/5 and 5/1 facet joints.
D. MRI before treatment.
E. MRI one year after treatment, showing significant reduction in hernia volume. - In Group A (lumbar region), very good outcomes (VG) were achieved in 46 cases, good outcomes (G) in 156 cases (VG + G = 202 cases, 91.4%), satisfactory (S) in 16 cases, and poor (P) in 3 cases (S + P = 19 cases, 8.6%).
- In Group B, very good results were obtained in 8 cases, good results in 29 cases (VG + G = 37 cases, 84%), satisfactory outcomes in 6 cases, and poor outcomes in 1 case (S + P = 7 cases, 16%).
- In Group C, results were very good in 2 cases, good in 7 cases (VG + G = 9 cases, 82%), satisfactory in 2 cases, and there were no poor outcomes (S + P = 2 cases, 18%).
- Only 2 cases of lumbar hernia with poor outcomes required surgical intervention: 1 in Group A and 1 in Group B.
- Improvement in patients was observed between 1 and 3 weeks after the procedure, except for 8 patients with acute hyperalgesic hernias, whose symptom improvement occurred within a day or the next day after the procedure.
- No allergic reactions occurred during or after the intradiscal injection of GEC. None of the patients developed infections. At the start of the injection, patients often reported slight discomfort in the area of the treated disc, which was explained by the injection speed, as this discomfort only occurs with rapid administration. The discomfort disappeared during the injection. No patients experienced acute lumbar pain during or after the procedure.
- FIGURE 3. Lumbar intervertebral disc hernia. The patient was asymptomatic before treatment; however, the MRI shows a hernia with reduced volume.
A. MRI before treatment.
B. MRI 3 months after treatment. - During the more than 4-year follow-up period of the first patients, no pathological events related to GEC treatment were identified.
- DISCUSSION
- We and some other specialists conclude that, when treating intervertebral disc hernias, therapeutic approaches that preserve spinal integrity should be preferred. Treatment with chymopapain nucleolysis has proven effective but has always been associated with the risk of allergic reactions (relatively rare but nevertheless undeniable) caused by this drug.¹²
- After the withdrawal of chymopapain from the market, alternative procedures were sought. Decompressive intradiscal procedures were used, such as disc vaporization during nucleoplasty with radiofrequency or mechanical reduction of disc pressure manually or using automated percutaneous diskectomy (APD).⁷⁸
- Nucleolysis with pure ethanol (PE) was proposed by Riquelme et al.,³ who demonstrated good results in treating lumbar intervertebral disc hernias.
- Our experience with PE confirmed its undeniable therapeutic effect, but its use is associated with certain inconveniences (for example, when applied in cervical or thoracic regions, or in hernias with epidural infiltration during discography, which we consider quite risky, as do Riquelme et al.,³ whose published work did not include such patients due to practically uncontrollable diffusion of the product). Moreover, some of our patients experienced acute radicular pain in the lower limb on the side of the disc puncture during PE injection, which resolved within days or weeks and was likely related to reflux of the substance onto the nerve root.
- FIGURE 4. Lumbar intervertebral disc hernia. The patient underwent an intradiscal injection of gelified ethanol with contrast (GEC). MRI shortly after the procedure and long-term follow-up.
A. MRI before treatment.
B. MRI 3 months after treatment, showing slight reduction in hernia volume; the patient is asymptomatic.
C. MRI 4 years after the procedure, with no visible hernia and stable good clinical result.
TABLE 3. Classification of outcomes
| Outcome Description | Abbreviation |
| No pain, no limitations, return to work | VG (Very Good) |
| Intermittent pain, minor limitations, return to work | G (Good) |
| Pain reduction, continued need for treatment, some limitations, return to work or not | S (Satisfactory) |
| No improvement or worsening pain, limited mobility, inability to return to work | P (Poor) |
Given the evident therapeutic effectiveness, we found it beneficial to enhance CE (Cauterizing Ethanol) through two modifications:
To improve control of the drug, we used a mixture of CE and ethylcellulose. We had previous experience using this mixture in the treatment of venous angiomas.⁴,⁵,⁹ Adding ethylcellulose results in a more viscous product that can be administered via a needle. Upon contact with the disc, it quickly turns into a substance resembling a piece of tissue soaked in alcohol in consistency. This modification creates a kind of intradiscal prosthesis, causing the product to remain within the disc, preventing it from leaking into the epidural space or onto the nerve root. This also ensures a more concentrated effect of CE, which stays in place with a minimal amount of the substance being injected.
To clearly register the injection performed, we added an inert metallic powder (tungsten or tantalum) to the product. Introducing a radiopaque powder into the disc allows for high-definition fluoroscopy, but the most interesting outcome is the disc-CT performed post-treatment: the topography of the gel is clearly visible. Apparently, the gel fills in weak zones and, in particular, intradiscal fissures (Figures 1, 2, 5, 6).
FIGURE 5. “Triple treatment” of a foraminal hernia (CEG, ACID, intra-articular steroid injections) provides a very good result.
A. CT before treatment.
B. Intradiscal treatment (CEG + ACID).
C. Intra-articular steroid injection.
D. CT after treatment. The CEG is concentrated in the hernia.
FIGURE 6. A 53-year-old woman with disabling radicular pain that forced her to leave work. After treatment at the levels identified via discography and following a positive clinical outcome, the patient returned to work.
A. MRI of the lumbar spine. The sagittal sequence shows several minimal disc bulges.
B. L2/L3 CT shows minimal right foraminal bulging.
C. L3/L4 CT shows left foraminal bulging.
D. Discography of the last three lumbar discs. All three discs are degenerated. Epidural infiltration is visible at the L3/L4 level. Pain is provoked only with contrast injection at L2/L3 and L3/L4. CEG injection was performed at L2/L3 and L3/L4.
E. Post-treatment disc-CT at L2/L3 level. CEG is visible in intradiscal fissures directed toward the right disc bulge and inside it.
F. Post-treatment disc-CT at L3/L4 level. CEG is visible in intradiscal fissures directed toward the left disc bulge and inside it.
In bulging hernias, gel penetration and concentration in the bulging fragment were usually (but not always) observed. The most intriguing post-treatment disc-CT findings were seen in patients with atypical symptoms, for whom standard imaging did not provide a complete anatomical explanation (Figure 6). By revealing various fissures in the disc, this drug allowed a different perspective on disc pathology. Given its good tolerability, it appears that this product can be administered at multiple levels during a single procedure in such cases.
With the use of CEG (Cauterizing Ethanol Gel), no immediate allergic complications or other types of pathological reactions were observed.
The product is easy to inject using a standard lumbar discography needle.
Treatment was performed on an outpatient basis, under local anesthesia or mild sedation. The acute radicular pain sometimes seen in patients treated with CE (liquid ethanol) did not occur. Only a few patients reported slight discomfort at the disc level at the beginning of the CEG injection (if the injection rate was too high). This may be related to the irritation of nerve endings in the disc at the onset of the therapeutic action; the sensation subsided during the injection and disappeared by the end of the procedure.
Due to the generally good clinical outcomes, MRI and CT were performed only in a few cases in this series, primarily to document anatomical changes in the disc. However, these cases were very illustrative.
MRI performed one year after treatment showed a significant reduction in the hernia volume (Figures 2C, 4D), but MRI performed a few weeks after treatment revealed a clear discrepancy between clinical symptoms and radiological findings: clinical symptoms could disappear even in the absence of changes in the herniated disc or with only minor changes (Figures 3I, 4I).
This confirms that the most important type of intradiscal therapeutic response is not the immediate reduction in hernia volume, but the reduction of intradiscal pressure: the disappearance of symptoms precedes the reduction of the hernia, which occurs only months or even years later.
We decided not to alter the protocol that was used with Chymopapain⁶, and systematically performed corticosteroid injections into adjacent facet joints in parallel.
The excessively high intradiscal pressure, treated through nucleolysis (or another intradiscal procedure), is accompanied by persistent inflammatory processes in surrounding tissues—and more importantly, in the facet joints—due to both mechanical and chemical factors. We know that such intra-articular injections improve the tolerance of intradiscal treatments and possibly the final outcome by more fully treating the pathological focus.
In conditions where Chymopapain was known to produce less favorable results—or where rapid pain relief was needed (e.g., foraminal hernias, spinal stenosis, hyperalgesic hernias) (Figure 5)—we used an additional intradiscal procedure (either ACID or RFN) to accelerate the therapeutic effect.
We termed this combination of two intradiscal procedures and an intra-articular corticosteroid injection a “triple treatment.”
The results obtained show that in such challenging cases, CEG can achieve outcomes as satisfactory as those obtained with triple treatment using Chymopapain.
RESULTS
We believe that this preliminary study has demonstrated that the effectiveness of the new substance in treating intervertebral disc herniations is comparable (based on our experience) to the effectiveness of Chymopapain.
In addition, its use has shown no allergic reactions or any other type of adverse reaction, both immediately after the procedure and over long-term observation—more than 4 years in the earliest cases.
While more evidence is needed to confirm the efficacy of CEG when used either alone or in combination with other procedures (such as intra-articular steroid injections, ACID, or RFN), and to establish its safety in other regions (e.g., cervical or thoracic spine), we believe that this study supports the feasibility of using CEG as a new form of percutaneous treatment for lumbar disc herniation.
BIBLIOGRAPHY
- Smith L. Chemonucleolysis. Personal history, trials, and tribulations. Clin Orthop Relat Res. 1993; 17–124.
- Smith L. Enzyme dissolution of the nucleus pulposus in humans. JAMA. 1964;187:137–140.
- Riquelme C, et al. Chemonucleolysis of lumbar disc herniation with ethanol. J Neuroradiol. 2001;28:219–229.
- Sunnier K, et al. A new sclerosing agent in the treatment of venous malformations. Study on 23 cases. Interven Neuroradiol. 2004;10:113–127.
- Tiret J, et al. Formulation of a sclerosing ethylcellulose alcoholic gel in the treatment of venous malformations. J Pharm Clin. 2001;20:12–16.
- Theron J. Percutaneous treatment of cervical and lumbar disc herniations, in Interventional Neuroradiology: Strategies and Practical Techniques. In: Connors JJ, Wojak JC, eds. Philadelphia: WB Saunders; 1999:424–430.
- Onik G, et al. Automated percutaneous diskectomy: initial patient experience. Work in progress. Radiology. 1987;162(1 Pt 1):129–132.
- Eggers P, Thapliyal H, Matthews L. Coblation: a newly described method for soft tissue surgery. Res Outcomes Arthrose Surg. 1997;2:1–4.
- Dompmartin A, et al. The use of an alcohol gel of ethyl cellulose in the treatment of venous malformations. Rev Stomatol Chir Maxillofac. 2000;101:30–32.