Spondylolisthesis is the displacement of one vertebra relative to the one below it. The displacement can be anterior (forward), posterior (backward), or lateral (to the side). The most common type is anterior spondylolisthesis.
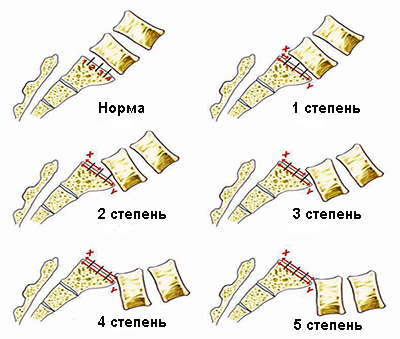
Classification of spondylolisthesis:
- Grade I: The posterior edge of the displaced vertebral body is within the bounds of the vertebra below.
- Grade II: Displacement is between 1/4 and 1/2 of the vertebral body width.
- Grade III: Displacement is between 1/2 and 3/4.
- Grade IV: Displacement ranges from 3/4 up to complete displacement.
- Grade V: Complete displacement of the vertebral body forward relative to the vertebra below (also called spondyloptosis).
There are two types of spondylolisthesis: unstable and stable. In unstable spondylolisthesis, the relative position of the displaced vertebra and the vertebra below changes with the patient’s posture. In stable spondylolisthesis, this positional relationship does not change.
The most common location of spondylolisthesis in children and adolescents is at the fifth lumbar vertebra (lumbosacral junction).
The occurrence of spondylolisthesis is caused by several factors, including:
- Congenital abnormal development of the lumbosacral region;
- Weakening of the ligamentous apparatus of the spine, which is a consequence of abnormal structure of the posterior spinal elements;
- Pathology of the intervertebral discs;
- Pathology of the facet joint region of the vertebral arch;
- Trauma and microtrauma;
- Disorders of metabolic and hormonal processes during various periods of postnatal human development;
- Hereditary predisposition.
Clinical presentation and diagnosis of spondylolisthesis:
The first painful symptoms of spondylolisthesis may not appear immediately after the onset of the pathology. Low back pain is observed in the vast majority of patients with spondylolisthesis, but the nature of the pain varies. Sometimes it is mild, sporadic pain or dull, constant pain. In other cases, the pain is sharp, often suddenly occurring after trauma, sudden movement, or lifting heavy objects.
The pain may remain acute for several days, then gradually subside at rest. After some time, the pain recurs and again passes relatively quickly, but over time the character changes: the pain becomes more intense, bothering the patient both at rest and when standing or moving, and worsens with bending forward and backward.
In spondylolisthesis of the fifth lumbar vertebra in children and adolescents, pain may initially appear in the legs. Pain in the lower limbs is a common sign of spondylolisthesis and is found in approximately 80% of patients. Sometimes this leg pain appears much earlier than back pain and serves as the first warning sign of a problem.
Increased lumbar lordosis is a consequence of the forward displacement of one of the lower lumbar vertebrae. This is especially noticeable in the early stages of the disease when the patient’s pelvis is in a normal position or even tilted forward.
Symptoms of urinary dysfunction may be present in some patients with spondylolisthesis. Transient weakness in the legs occurs when patients cannot walk for a long time without stopping due to a feeling of weakness in one or both legs. At rest, sitting or standing briefly is enough to restore leg strength. The cause of transient leg weakness is related to sudden onset and rapid resolution of spinal cord ischemia.

Diagnosis
With modern diagnostic methods, the diagnosis of spondylolysis can be made with complete certainty. Radiographic diagnosis of pronounced forms of spondylolisthesis does not present significant difficulties, although diagnostic errors still occur.
It is more challenging to diagnose the early stages of the pathological process, and timely detection in children and adolescents is crucial. Spondylolisthesis is characterized by a number of direct radiological signs by which the disease can be diagnosed without error. Lateral projection X-rays are primary in diagnosing spondylolisthesis. These should be taken in positions of trunk flexion and extension, allowing evaluation of stability at the vertebral displacement level.
A direct sign of spondylolisthesis is the symptom of anterior displacement of the vertebral body. Computed tomography (CT) and magnetic resonance imaging (MRI) should be used to study the condition of the spinal canal and intervertebral discs at the vertebral displacement level.
Prevention of Spondylolisthesis
Prevention in childhood involves early identification of children showing signs of the disease. Pigmented or depigmented spots, and increased hair growth in the lumbosacral region are external manifestations of possible dysplasia of the lumbosacral spine. It is also necessary to identify children with postural abnormalities as early as possible, particularly those with pathologically deep lumbar lordosis often accompanied by increased thoracic kyphosis, as well as children with lumbar scoliosis. These children should undergo thorough radiological examination. If pronounced abnormal development of the lumbosacral spine is detected, they must be placed under medical supervision.
Strengthening the muscular system, promoting correct posture, and avoiding sports with a risk of injury are fundamental to preventing spondylolisthesis in children and adolescents.
Therapeutic Exercise
Therapeutic exercise is an important treatment method in conservative management of spondylolisthesis. The exercise program includes movements that reduce lumbar lordosis. Exercises are recommended on the back, on a Swedish wall ladder, inclined plane, or in a semi-kneeling position on hands and knees.
Braces
Braces are among the most effective conservative treatment tools for spondylolisthesis and can sometimes quickly improve the patient’s condition.
Surgical Treatment of Spondylolisthesis
Indications for surgery depend on the clinical picture (especially neurological symptoms), patient age, cause of spondylolisthesis, stability and degree of vertebral displacement, and its location.
Absolute indications for surgery in children and adolescents with spondylolisthesis are:
- Presence of progressive spondylolisthesis of grades II–IV;
- Presence of pronounced neurological symptoms;
- Combination of progressive scoliosis with progressive spondylolisthesis;
- Progressive spondylolisthesis with significant lumbosacral spine abnormality;
- Traumatic spondylolisthesis.
The choice of surgical method depends on the degree of vertebral displacement and the clinical presentation. The main goal of surgery is to stabilize the displaced vertebra by creating a bone block. Anterior, posterior, and combined stabilization methods (spinal fusion) are used. Surgical tactics are determined individually for each case.
Case Example
X-rays of a 15-year-old patient diagnosed with unstable grade 3 spondylolisthesis of the 5th lumbar vertebra, presenting with lumbosciatica (leg pain) and pelvic organ dysfunction.
The CT scan of the same patient shows a zone of spondylolysis of the vertebral arch and narrowing of the spinal canal at the level of displacement.
The patient underwent surgery: decompressive laminectomy at the level of the 5th lumbar and 1st sacral vertebrae, reduction, posterior fixation with a metal construct, and posterior spinal fusion (spondylodesis).
On the follow-up X-ray, the reduction is maintained. On the follow-up CT scan, fusion of the spondylolysis zone is observed. Neurological symptoms are absent.