Scoliotic disease is a genetically determined disorder of the human musculoskeletal system, characterized by a multi-planar deformation of the spine, rib cage, and pelvis. It is accompanied by impaired function of the body’s organs and systems and causes severe physical and emotional suffering, leading to early disability and a significant reduction in life expectancy.
Scoliosis is among the most complex problems in modern orthopedics. According to literature data, the prevalence of scoliosis among the pediatric population is 5-9% (Charles Y.P., Daures J.-P., de Rosa V., 2006).
According to epidemiological studies conducted by the Research Institute of Traumatology and Orthopedics (Research Institute TsZMR) in 2000, the prevalence of scoliosis in the Republic of Moldova reaches 5.2% within the structure of musculoskeletal diseases. Research data indicate that the average life expectancy of untreated patients with severe forms of scoliotic disease does not exceed 35-40 years (Kralin A.B. 2003, Nazon D., Abergel G., 2003, Shimizu K; Hirakata M. 2006, Everett C.R., Patel R.K. 2007).
A characteristic feature of scoliosis is progression, which is associated with the age and growth of the child.
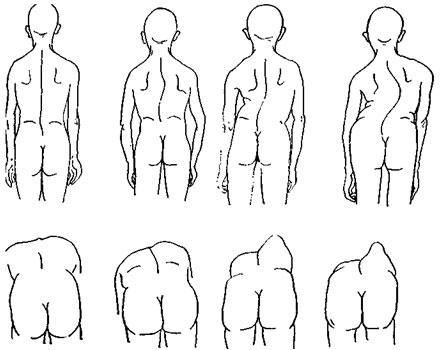
Orthopedic doctors distinguish 4 stages of scoliosis development:
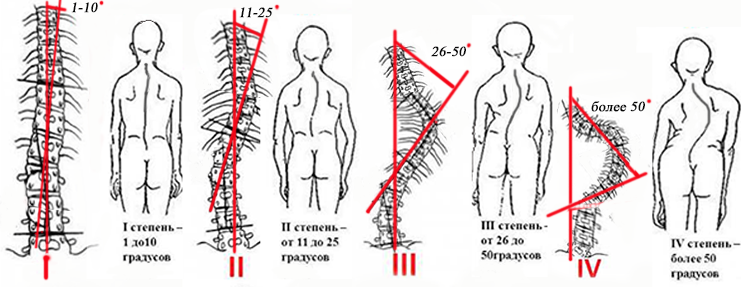
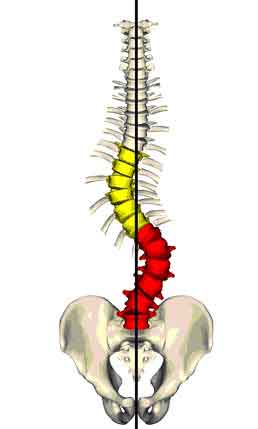
Stage 1: Curve angle does not exceed 10 degrees.
This stage is the hardest to diagnose. The patient feels no pain and does not notice posture changes. Detecting the curvature so early can be considered very fortunate. Treatment at this stage consists of massage, therapeutic physical exercises, and wearing a brace for a few hours per day (usually at night). Conservative methods at this stage have a positive effect in 99% of cases.
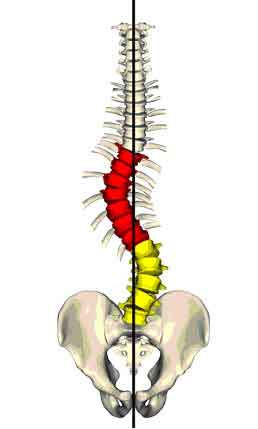
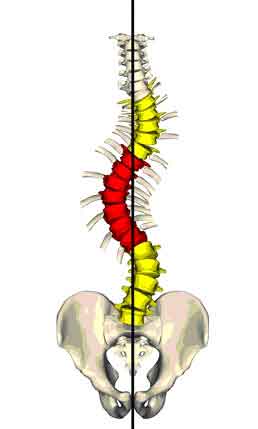
Stage 2: Curve angle from 10 to 25 degrees.
The second curve is just beginning to form; scapular asymmetry becomes visible when bending forward. Correcting the spinal curvature is possible in about 80% of cases. The patient is prescribed massage, a set of physical exercises, and corset therapy. There is no pain, so no medications are prescribed.
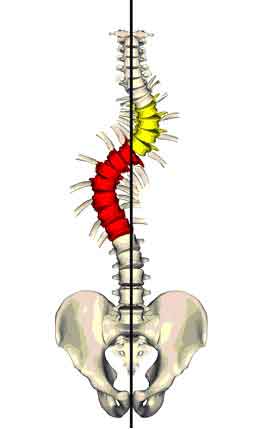
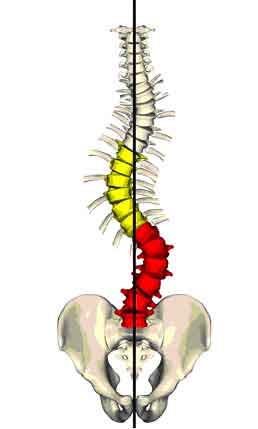
Stage 3: Angle from 25 to 50 degrees.
A severe form. In addition to scapular asymmetry there appears a rib hump, which is clearly visible from the side. The deformation starts to affect the function of the rib cage, respiratory organs, and the cardiovascular system. The patient is required to wear a brace for at least 16 hours a day. Treatment of stage 3 scoliosis implies comprehensive therapy: swimming, physical therapy, manual procedures, massage. Sometimes pain-relieving medication is needed. In severe cases, the doctor may decide on surgery.
Stage 4: The most severe — curve angle over 50 degrees.
Several types of scoliosis are distinguished:
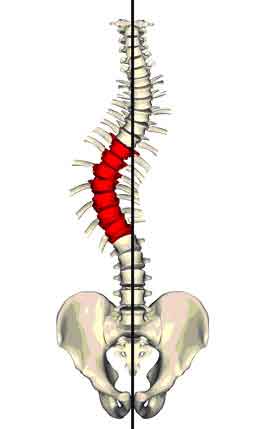
- Lumbar
- Cervical
- Thoracic
- In some cases, combined
By patient’s age scoliosis is divided into categories:
- Infantile (patients under 3 years old)
- Juvenile (3–10 years)
- Adolescent (10–15 years)
- Adult
Forms of scoliosis by etiology and pathogenesis:
- Congenital (including dysplastic and idiopathic)
- Neurogenic
- Static
Congenital scoliosis is caused by deformities arising from changes in the spinal skeletal structure: rib fusion on one side, extra ribs and hemivertebrae, synostosis of spinous processes, defects in the vertebral arches, dysplasia of the lumbosacral area.
Dysplastic scoliosis develops due to anomalies in vertebral development (spondylolysis, failure of vertebral arches to close, unilateral sacralization or lumbarization). Because of shared congenital origins, many combine congenital and dysplastic forms under one category.
Idiopathic scoliosis — the most common form — but its origins remain not fully understood. Some biochemical findings suggest hormonal factors. Many authors note disturbance of neuromuscular balance or some neuro-dystrophic processes (especially in muscle tissue) of congenital character. Thus, many researchers classify idiopathic scoliosis alongside dysplastic and congenital scoliosis.
Neurogenic scoliosis mostly arises from prior poliomyelitis and is caused by imbalance in the back muscles and oblique abdominal muscles. Neurogenic scoliosis also includes cases arising from myopathy, syringomyelia, neurofibromatosis, spastic paralysis, etc.
Static scoliosis most often arises as a result of disorders of a lower limb joint (ankylosis, congenital hip dislocation, etc.), accompanied by shortening of the limb and subsequent persistent changes in the spine.
Forms of curvature by clinical course:
Based on how quickly the disease progresses, two categories are used:
- Progressive
- Non-progressive
- Slowly progressive: increase of curvature angle up to 9 degrees per year
- Rapidly progressive: increase of curvature angle of 10 degrees or more per year
Radiological signs are used to determine the degree of scoliosis progression.
Degree by severity of deformation (J.I.P. James, 1954; J.R. Cobb angle, 1948)
- 0–69° — mild degree
- 37–98° — severe degree
- 100° — very severe degree
By change of deformation depending on load on the spine:
- Non-fixed (unstable) scoliosis
- Fixed (stable) scoliosis
By curve variant (Lenke classification, L.G. Lenke, 2006)
In Lenke classification there are three subcategories used for diagnosis.
- TYPES OF SCOLIOTIC CURVES
II. LUMBAR MODIFIER
The lumbar modifier is determined by identifying the position of the most laterally displaced vertebra in relation to the Central Sacral Vertical Line (CSVL).
- Lumbar Modifier A – The CSVL passes between the pedicles of L1–L4.
- Lumbar Modifier B – The CSVL touches the pedicle of the apical vertebra (L1–L4).
- Lumbar Modifier C – The CSVL is located medial to the apical vertebra.
III. THORACIC SAGITTAL MODIFIER
The thoracic sagittal modifier is based on the Cobb angle measured between the superior endplate of T5 and the inferior endplate of T12 on a lateral radiograph.
- Hypokyphosis (–): Angle less than +10°, or lordosis
- Normokyphosis (N): Angle between +10° and +40°
- Hyperkyphosis (+): Angle greater than +40°
USE OF THE LENKE CLASSIFICATION
The Lenke classification includes the Curve Type (Types 1–6), Lumbar Modifier (A, B, or C), and, from the lateral radiograph, the Thoracic Sagittal Modifier (–, N, +).
For example: 1A–.